A Person Who Delivers Babys Is Called Obstetrician Common Major in College
| | Expect upwardly obstetrics in Wiktionary, the complimentary dictionary. |
| Occupation | |
|---|---|
| Names |
|
| Occupation type | Specialty |
| Activity sectors | Medicine, surgery |
| Description | |
| Pedagogy required |
|
| Fields of | Hospitals, clinics |
Obstetrics is the subject concentrated on pregnancy, childbirth and the postpartum period. As a medical specialty, obstetrics is combined with gynecology under the discipline known every bit obstetrics and gynecology (OB/GYN), which is a surgical field.[1]
Principal areas [edit]
Prenatal care [edit]
Prenatal care is important in screening for various complications of pregnancy. This includes routine office visits with physical exams and routine lab tests:
-

Fetus at 17 weeks
-

Fetus at xx weeks
First trimester [edit]
Routine tests in the start trimester of pregnancy mostly include:
- Complete blood count
- Blood type
- Rh-negative antenatal patients should receive RhoGAM at 28 weeks to preclude Rh illness.
- Indirect Coombs exam (AGT) to assess run a risk of hemolytic disease of the newborn
- Rapid plasma reagin examination to screen for syphilis
- Rubella antibody screen
- HBsAg test to screen for hepatitis B
- Testing for chlamydia (and gonorrhea when indicated)
- Mantoux test for tuberculosis
- Urinalysis and culture
- HIV screen
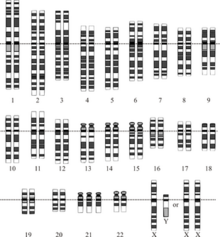
Genetic screening for Down syndrome (trisomy 21) and Edwards syndrome (trisomy eighteen), the national standard in the U.s.a., is rapidly evolving away from the AFP-quad screen, done typically in the second trimester at 16–18 weeks. The newer integrated screen (formerly called F.A.South.T.E.R for Start And Second Trimester Early Results) can be done at 10 plus weeks to 13 plus weeks with an ultrasound of the fetal neck (thicker nuchal skin correlates with higher risk of Down syndrome existence present) and two chemicals (analytes), pregnancy-associated plasma protein A and human chorionic gonadotropin (pregnancy hormone level itself). It gives an accurate take chances profile very early. A second blood screen at xv to 20 weeks refines the take chances more accurately. The cost is college than an "AFP-quad" screen due to the ultrasound and second blood test, but it is quoted to accept a 93% pick upwards rate as opposed to 88% for the standard AFP/QS. This is an evolving standard of intendance in the United States.[2] [3] [ citation needed ]
Second trimester [edit]
- MSAFP/quad. screen (4 simultaneous claret tests) (maternal serum AFP, inhibin A, estriol, & βHCG) – elevations, depression numbers or odd patterns correlate with neural tube defect run a risk and increased risks of trisomy 18 or trisomy 21
- Ultrasound either intestinal or transvaginal to assess neck, placenta, fluid and baby
- Amniocentesis is the national standard (in what country) for women over 35 or who attain 35 by mid pregnancy or who are at increased run a risk by family history or prior nascency history.
Tertiary trimester [edit]
- Hematocrit (if low, the mother receives fe supplements)
- Group B Streptococcus screen. If positive, the woman receives 4 penicillin or ampicillin while in labor—or, if she is allergic to penicillin, an culling therapy, such every bit 4 clindamycin or IV vancomycin.
- Glucose loading test (GLT) – screens for gestational diabetes; if > 140 mg/dL, a glucose tolerance test (GTT) is administered; a fasting glucose > 105 mg/dL suggests gestational diabetes.
About doctors practise a sugar load in a drink class of fifty grams of glucose in cola, lime or orangish and depict blood an hour later (plus or minus 5 minutes). The standard modified criteria accept been lowered to 135 since the late 1980s.

The issue of an Ultrasonography: a black and white image that shows a clear view of the interior abdomen.
Fetal assessments [edit]

A dating scan at 12 weeks.
Obstetric ultrasonography is routinely used for dating the gestational historic period of a pregnancy from the size of the fetus, determine the number of fetuses and placentae, evaluate for an ectopic pregnancy and starting time trimester bleeding, the nigh authentic dating being in showtime trimester before the growth of the foetus has been significantly influenced by other factors. Ultrasound is too used for detecting congenital anomalies (or other foetal anomalies) and determining the biophysical profiles (BPP), which are more often than not easier to detect in the 2nd trimester when the foetal structures are larger and more adult. Specialised ultrasound equipment can also evaluate the claret flow velocity in the umbilical string, looking to detect a decrease/absenteeism/reversal or diastolic blood flow in the umbilical artery.
X-rays and computerized tomography (CT) are non used, peculiarly in the first trimester, due to the ionizing radiation, which has teratogenic furnishings on the foetus. No furnishings of magnetic resonance imaging (MRI) on the foetus have been demonstrated,[4] but this technique is besides expensive for routine ascertainment. Instead, obstetric ultrasonography is the imaging method of choice in the starting time trimester and throughout the pregnancy, because information technology emits no radiations, is portable, and allows for realtime imaging.
The safety of frequent ultrasound scanning has not been confirmed. Despite this, increasing numbers of women are choosing to accept additional scans for no medical purpose, such as gender scans, 3D and 4D scans. A normal gestation would reveal a gestational sac, yolk sac, and fetal pole. The gestational age can be assessed by evaluating the mean gestational sac diameter (MGD) before week vi, and the crown-rump length later on week 6. Multiple gestation is evaluated by the number of placentae and amniotic sacs nowadays.
Other tools used for assessment include:
- Fetal screening is used to help assess the viability of the fetus, too as congenital abnormalities.
- Fetal karyotype tin can be used for the screening of genetic diseases. This tin can be obtained via amniocentesis or chorionic villus sampling (CVS)
- Foetal haematocrit for the cess of foetal anemia, Rh isoimmunization, or hydrops tin be determined by percutaneous umbilical blood sampling (PUBS), which is done by placing a needle through the abdomen into the uterus and taking a portion of the umbilical cord.
- Fetal lung maturity is associated with how much surfactant the fetus is producing. Reduced product of surfactant indicates decreased lung maturity and is a loftier run a risk factor for babe respiratory distress syndrome. Typically a lecithin:sphingomyelin ratio greater than ane.5 is associated with increased lung maturity.
- Nonstress test (NST) for fetal heart rate
- Oxytocin challenge test
Diseases in pregnancy [edit]
A significant woman may have a pre-existing illness, that may become worse or become a risk to the pregnancy, or to postnatal developmentthe offspring
- Diabetes mellitus and pregnancy deals with the interactions of diabetes mellitus (not restricted to gestational diabetes) and pregnancy. Risks for the child include miscarriage, growth restriction, growth acceleration, foetal obesity (macrosomia), polyhydramnios and birth defects.
- Lupus and pregnancy confers an increased rate of foetal death in utero and spontaneous abortion (miscarriage), every bit well as of neonatal lupus.
- Thyroid disease in pregnancy can, if uncorrected, cause agin effects on foetal and maternal well-existence. The deleterious effects of thyroid dysfunction can also extend beyond pregnancy and delivery to affect neurointellectual development in the early life of the child. Need for thyroid hormones is increased during pregnancy, and may cause a previously unnoticed thyroid disorder to worsen.
- Hypercoagulability in pregnancy is the propensity of pregnant women to develop thrombosis (blood clots). Pregnancy itself is a gene of hypercoagulability (pregnancy-induced hypercoagulability), as a physiologically adaptive mechanism to prevent postal service partum bleeding.[5] Yet, when combined with an additional underlying hypercoagulable states, the risk of thrombosis or embolism may become substantial.[v]
Induction and labour [edit]
Induction is a method of artificially or prematurely stimulating labour in a woman. Reasons to induce can include pre-eclampsia, foetal distress, placental malfunction, intrauterine growth retardation and failure to progress through labour increasing the hazard of infection and foetal distresses.
Induction may exist achieved via several methods:
- Disturbance of cervical membranes
- Pessary of Prostin foam, prostaglandin E2
- Intravaginal or oral assistants of misoprostol
- Cervical insertion of a 30-mL Foley catheter
- Rupturing the amniotic membranes
- Intravenous infusion of synthetic oxytocin (Pitocin or Syntocinon)
During labour, the obstetrician carries out the following tasks:
- Monitor the progress of labour, by reviewing the nursing chart, performing vaginal examination, and assessing the trace produced by a foetal monitoring device (the cardiotocograph)
- Provide hurting relief, either by nitrous oxide, opiates, or past epidural amazement done by anaesthestists, an anaesthesiologist, or a nurse anaesthetist.
- Caesarean section, if there is an associated risk with vaginal delivery, as such foetal or maternal compromise.
Complications and emergencies [edit]
The main emergencies include:
- Ectopic pregnancy is when an embryo implants in the uterine (Fallopian) tube or (rarely) on the ovary or within the peritoneal cavity. This may cause massive internal bleeding.
- Pre-eclampsia is a illness divers by a combination of signs and symptoms that are related to maternal hypertension. The cause is unknown, and markers are existence sought to predict its development from the primeval stages of pregnancy. Some unknown factors crusade vascular harm in the endothelium, causing hypertension. If severe, it progresses to eclampsia, where seizures occur, which can be fatal. Preeclamptic patients with the HELLP syndrome show liver failure and Disseminated intravascular coagulation (DIC). The but handling is to evangelize the foetus. Women may still develop pre-eclampsia post-obit delivery.
- Placental abruption is where the placenta detaches from the uterus and the adult female and foetus can drain to death if non managed appropriately.
- Foetal distress where the foetus is getting compromised in the uterine environment.
- Shoulder dystocia where 1 of the foetus' shoulders becomes stuck during vaginal birth. There are many risk factors, including macrosmic (large) foetus, simply many are also unexplained.
- Uterine rupture can occur during obstructed labour and endanger foetal and maternal life.
- Prolapsed cord tin can merely happen after the membranes have ruptured. The umbilical cord delivers before the presenting office of the foetus. If the foetus is not delivered inside minutes, or the pressure taken off the cord, the foetus dies.
- Obstetrical hemorrhage may be due to a number of factors such as placenta previa, uterine rupture or tears, uterine atony, retained placenta or placental fragments, or bleeding disorders.
- Puerperal sepsis is an ascending infection of the genital tract. It may happen during or afterwards labour. Signs to look out for include signs of infection (pyrexia or hypothermia, raised heart rate and respiratory rate, reduced blood pressure), and abdominal pain, offensive lochia (blood loss) increased lochia, clots, diarrhea and vomiting.
Postpartum menses [edit]
The World Health Arrangement makes a distinction betwixt the utilize of postpartum care when it concerns the care of the mother after giving birth, and postnatal care when the care of the newborn is concerned.[6] Postpartum care is provided to the mother post-obit childbirth.
A woman in the Western globe who gives nascence in a hospital may leave the hospital as before long every bit she is medically stable, and chooses to leave, which can be as early as a few hours later, just commonly averages a stay of one or two days; the average postnatal stay post-obit delivery by caesarean department is 3 to four days.
During this time the mother is monitored for haemorrhage, bowel and float role, and infant care. The infant'southward health is besides monitored.
Veterinarian obstetrics [edit]
History [edit]
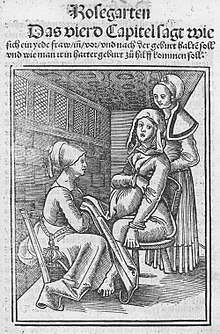
Prior to the 18th century, caring for pregnant women in Europe was confined exclusively to women, and rigorously excluded men. The expectant female parent would invite close female friends and family members to her home to go on her visitor during childbirth.[7] Skilled midwives managed all aspects of the labour and delivery. The presence of physicians and surgeons was very rare and just occurred if a serious complication had taken place and the midwife had exhausted all measures at her disposal. Calling a surgeon was very much a last resort and having men deliver women in this era was seen as offending female modesty.[viii] [ix]
Before the 18th century [edit]
Prior to the 18th and 19th centuries, midwifery was well established only obstetrics was not recognized as a specific medical specialty. However, the discipline matter and interest in the female reproductive organization and sexual practice can be traced back to Ancient Egypt[ten] and Ancient Greece.[11] Soranus of Ephesus sometimes is called the near important effigy in ancient gynecology. Living in the late outset century A.D. and early on second century, he studied beefcake and had opinions and techniques on abortion, contraception –virtually notably coitus interruptus– and birth complications. After his death, techniques and works of gynecology declined; very little of his works were recorded and survived to the late 18th century when gynecology and obstetrics reemerged every bit a medical specialism.[12]
18th century [edit]
The 18th century marked the beginning of many advances in European midwifery, based on improve noesis of the physiology of pregnancy and labour. Past the end of the century, medical professionals began to understand the anatomy of the uterus and the physiological changes that take identify during labour. The introduction of forceps in childbirth also took place at this time. All these medical advances in obstetrics were a lever for the introduction of men into an loonshit previously managed and run by women—midwifery.[thirteen]
The add-on of the male person-midwife (or man-midwife) is historically a significant change to the profession of obstetrics. In the 18th century medical men began to train in area of childbirth and believed with their advanced cognition in beefcake that childbirth could be improved. In France these male-midwives were referred to every bit accoucheurs, a title afterward used all over Europe. The founding of lying-in hospitals besides contributed to the medicalization and male-dominance of obstetrics. These early motherhood hospitals were establishments where women would come to accept their babies delivered, as opposed to the practise since time immemorial of the midwife attention the dwelling house of the adult female in labour. This establishment provided male-midwives with countless patients to practice their techniques on and was a way for these men to demonstrate their noesis.[14]
Many midwives of the time bitterly opposed the involvement of men in childbirth. Some male person practitioners also opposed the involvement of medical men like themselves in midwifery and even went as far as to say that male-midwives but undertook midwifery solely for perverse erotic satisfaction. The accoucheurs argued that their interest in midwifery was to improve the procedure of childbirth. These men too believed that obstetrics would forge ahead and continue to strengthen.[eight]
19th century [edit]
18th-century physicians expected that obstetrics would continue to grow, just the opposite happened. Obstetrics entered a stage of stagnation in the 19th century, which lasted until about the 1880s.[7] The central explanation for the lack of advancement during this time was the rejection of obstetrics by the medical community. The 19th century marked an era of medical reform in Europe and increased regulation over the profession. Major European institutions such every bit The College of Physicians and Surgeons[ where? ] considered delivering babies ungentlemanly work and refused to have anything to practice with childbirth as a whole. Even when Medical Act 1858 was introduced, which stated that medical students could qualify as doctors, midwifery was entirely ignored. This made it almost incommunicable to pursue an education in midwifery and as well take the recognition of being a doc or surgeon. Obstetrics was pushed to the side.[15]
By the belatedly 19th century, the foundation of modern-twenty-four hour period obstetrics and midwifery began developing. Delivery of babies past doctors became pop and readily accepted, only midwives continued to play a part in childbirth. Midwifery also changed during this era due to increased regulation and the eventual need for midwives to get certified. Many European countries past the tardily 19th century were monitoring the training of midwives and issued certification based on competency. Midwives were no longer uneducated in the formal sense.[16]
As midwifery began to develop, and then did the profession of obstetrics near the end of the century. Childbirth was no longer unjustifiably despised by the medical community equally it in one case had been at the first of the century. Just obstetrics was underdeveloped compared to other medical specialities. Many male person physicians would deliver children but very few would have referred to themselves as obstetricians. The end of the 19th century did mark a significant accomplishment in the profession with the advancements in asepsis and anaesthesia, which paved the style for the mainstream introduction and after success of the Caesarean Department.[16] [17]
Before the 1880s mortality rates in lying-hospitals would reach unacceptably high levels and became an area of public business organization. Much of these maternal deaths were due to puerperal fever, so known as childbed fever. In the 1800s Dr. Ignaz Semmelweis noticed that women giving nascency at home had a much lower incidence of childbed fever than those giving nascency past physicians in lying-hospitals. His investigation discovered that washing easily with an clarified solution before a delivery reduced childbed fever fatalities by 90%.[18] So it was ended that it was physicians who had been spreading disease from ane labouring mother to the next. Despite the publication of this data, doctors all the same would not wash. It was not until the 20th century when advancements in aseptic technique and the understanding of disease would play a significant function in the decrease of maternal mortality rates among many populations.
History of obstetrics in America [edit]
The development of obstetrics every bit a practice for accredited doctors happened at the plough of the 18th century and thus was very differently developed in Europe and in the Americas due to the independence of many countries in the Americas from European powers. "Unlike in Europe and the British Isles, where midwifery laws were national, in America, midwifery laws were local and varied widely".[19]
Gynaecology and Obstetrics gained attention in the American medical field at the end of the nineteenth century through the evolution of such procedures as the ovariotomy. These procedures and so were shared with European surgeons who replicated the surgeries. This was a period when antiseptic, aseptic or anaesthetic measures were just being introduced to surgical and observational procedures and without these procedures surgeries were dangerous and often fatal. Following are 2 surgeons noted for their contributions to these fields include Ephraim McDowell and James Marion Sims.
Ephraim McDowell adult a surgical practice in 1795 and performed the first ovariotomy in 1809 on a 47-year-old widow who then lived on for xxx-one more years. He had attempted to share this with John Bell whom he had practiced under who had retired to Italian republic. Bong was said to have died without seeing the document but information technology was published by an associate in Extractions of Diseased Ovaria in 1825. By the mid-century the surgery was both successfully and unsuccessfully being performed. Pennsylvanian surgeons the Attlee brothers made this process very routine for a full of 465 surgeries–John Attlee performed 64 successfully of 78 while his blood brother William reported 387– between the years of 1843 and 1883. By the centre of the nineteenth century this procedure was successfully performed in Europe by English surgeons Sir Spencer Wells and Charles Clay every bit well as French surgeons Eugène Koeberlé, Auguste Nélaton and Jules Péan.[20]
J. Marion Sims was the surgeon responsible for existence the first treating a vesicovaginal fistula[20]–a condition linked to many caused mainly past prolonged pressing of the foetus against the pelvis or other causes such as rape, hysterectomy, or other operations– and also having been physician to many European royals and the 20th President of the United States James A. Garfield subsequently he had been shot. Sims does take a controversial medical by. Under the beliefs at the fourth dimension about pain and the prejudice towards African people, he had skillful his surgical skills and developed skills on slaves.[21] These women were the first patients of modern gynecology. One of the women he operated on was named Anarcha Westcott, the woman he first treated for a fistula.[22]
Historical role of gender [edit]
Women and men inhabited very different roles in natal intendance upwards to the 18th century. The role of a dr. was exclusively held by men who went to academy, an overly male establishment, who would theorize beefcake and the process of reproduction based on theological teaching and philosophy. Many beliefs about the female trunk and catamenia in the 17th and 18th centuries were inaccurate; clearly resulting from the lack of literature nigh the practice.[23] Many of the theories of what caused menses prevailed from Hippocratic philosophy.[24] Midwives of this time were those assisted in the birth and intendance of both born and unborn children, and as the name suggests, this position was held mainly past women.
During the nativity of a child, men were rarely present. Women from the neighbourhood or family unit would join in on the process of nascency and assist in many different means. The one position where men would help with the birth of a child would be in the sitting position, usually when performed on the side of a bed to support the mother.[25]
Men were introduced into the field of obstetrics in the nineteenth century and resulted in a change of the focus of this profession. Gynaecology directly resulted as a new and separate field of study from obstetrics and focused on the curing of illness and indispositions of female person sexual organs. This had some relevance to some conditions every bit menopause, uterine and cervical bug, and childbirth could leave the mother in need of extensive surgery to repair tissue. But, at that place was also a large arraign of the uterus for completely unrelated conditions. This led to many social consequences of the nineteenth century.[23]
Come across also [edit]
| | Wikimedia Commons has media related to Obstetrics. |
- Henry Jacques Garrigues, who introduced antiseptic obstetrics to Northward America
- Maternal-fetal medicine
- Obstetrical nursing
References [edit]
- ^ "Obstetrics and Gynecology Specialty Description". American Medical Association. Retrieved 24 October 2020.
- ^ Carlson, Laura M.; Vora, Neeta Fifty. (2017). "Prenatal Diagnosis". Obstetrics and Gynecology Clinics of North America. 44 (two): 245–256. doi:10.1016/j.ogc.2017.02.004. PMC5548328. PMID 28499534.
- ^ Zhang, Wei (2019). "Cost-effectiveness of prenatal screening and diagnostic strategies for Down's syndrome: A microsimulation modeling assay". PLOS ONE. 14 (12): e0225281. Bibcode:2019PLoSO..1425281Z. doi:ten.1371/journal.pone.0225281. PMC6892535. PMID 31800591.
- ^ Ibrahim A. Alorainy; Fahad B. Albadr; Abdullah H. Abujamea (2006). "Attitude towards MRI prophylactic during pregnancy". Ann Saudi Med. 26 (4): 306–9. doi:10.5144/0256-4947.2006.306. PMC6074503. PMID 16885635.
- ^ a b Page 264 in: Gresele, Paolo (2008). Platelets in haematologic and cardiovascular disorders: a clinical handbook. Cambridge, Britain: Cambridge Academy Printing. ISBN978-0-521-88115-nine.
- ^ Information, National Center for Biotechnology; Pike, U. S. National Library of Medicine 8600 Rockville; MD, Bethesda; Usa, Bethesda (2010). "WHO Technical Consultation on Postpartum Care". World Wellness Organization. Retrieved xxx June 2020.
- ^ a b Gelis, Jacques. History of Childbirth. Boston: Northeastern University Printing, 1991: 96–98
- ^ a b Bynum, W.F., & Porter, Roy, eds. Companion Encyclopedia of the History of Medicine. London and New York: Routledge, 1993: 1050–1051.
- ^ Carr, Ian., "Academy of Manitoba: Women'south Health." May 2000, accessed May 20, 2012, http://www.neonatology.org/pdf/dyingtohaveababy.pdf
- ^ McGrew, Roderick Eastward. Encyclopedia of Medical History. New York: McGraw-Hill Volume Visitor, 1985. 122.
- ^ Hufnagel, Glenda Lewin. A History of Women's Menstruation from Aboriginal Greece to the 20-Starting time Century: Psychological, Social, Medical, Religious, and Educational Issues. Lewiston: Edwin Mellen Printing, 2012. xv.
- ^ McGrew, Roderick E. Encyclopedia of Medical History. New York: McGraw-Hill Book Visitor, 1985. 123.
- ^ Bynum, Westward.F., & Porter, Roy, eds. Companion Encyclopedia of the History of Medicine. London and New York: Routledge, 1993: 1051–1052.
- ^ Martell, Louise K. (2000). "The Hospital and the Postpartum Experience: A Historical Assay". Periodical of Obstetric, Gynecologic, and Neonatal Nursing. 29 (1): 65–72. doi:10.1111/j.1552-6909.2000.tb02757.10. PMID 10660278. Retrieved 27 October 2020.
- ^ Bynum, W.F., & Porter, Roy, eds. Companion Encyclopedia of the History of Medicine. London and New York: Routledge, 1993: 1053–1055.
- ^ a b Drife, James, "The outset of life: a history of obstetrics," Postgraduate Medical Journal 78 (2002): 311–315, accessed May 21, 2012. doi:10.1136/pmj.78.919.311.
- ^ Low, James., "Caesarean department-past and nowadays," Journal of obstetrics and gynecology Canada 31, no. 12 (2009): 1131–1136, accessed May 20, 2012. http://www.sogc.org/jogc/abstracts/total/200912_Obstetrics_2.pdf Archived 2013-01-23 at the Wayback Auto
- ^ Caplan, Caralee E. (1995). "The Childbed Fever Mystery and the Meaning of Medical Journalism". McGill Journal of Medicine. 1 (ane). Archived from the original on 2012-07-07.
- ^ Roth, Judith. "Pregnancy & Nativity: The History of Childbearing Choices in the United states."Homo Service Solutions. Accessed February 14th, 2014. http://world wide web.ourbodiesourselves.org/
- ^ a b McGrew, Roderick Eastward. Encyclopedia of Medical History. New York: McGraw-Hill Book Company, 1985. 125.
- ^ International Wellness Foundation." Dr. J Marion Sims: The Begetter of Modern Gynecology." February 12th, 2014. world wide web.mnwelldir.org/docs/history/biographies/marion_sims.htm
- ^ International Wellness Foundation. "Anarcha The Mother of Gynaecology." March 28th, 2014. www.mnwelldir.org/docs/history/biographies/marion_sims.htm
- ^ a b McGrew, Roderick Eastward. Encyclopedia of Medical History. New York: McGraw-Hill Volume Company, 1985. 123–125.
- ^ Hufnagel, Glenda Lewin. A History of Women'southward Menstruation from Ancient Greece to the Twenty-First Century: Psychological, Social, Medical, Religious, and Educational Issues. Lewiston: Edwin Mellen Press, 2012. sixteen.
- ^ Gelis, Jacques. History of Childbirth. Boston: Northeastern University Press, 1991: 130.
Source: https://en.wikipedia.org/wiki/Obstetrics
0 Response to "A Person Who Delivers Babys Is Called Obstetrician Common Major in College"
Post a Comment